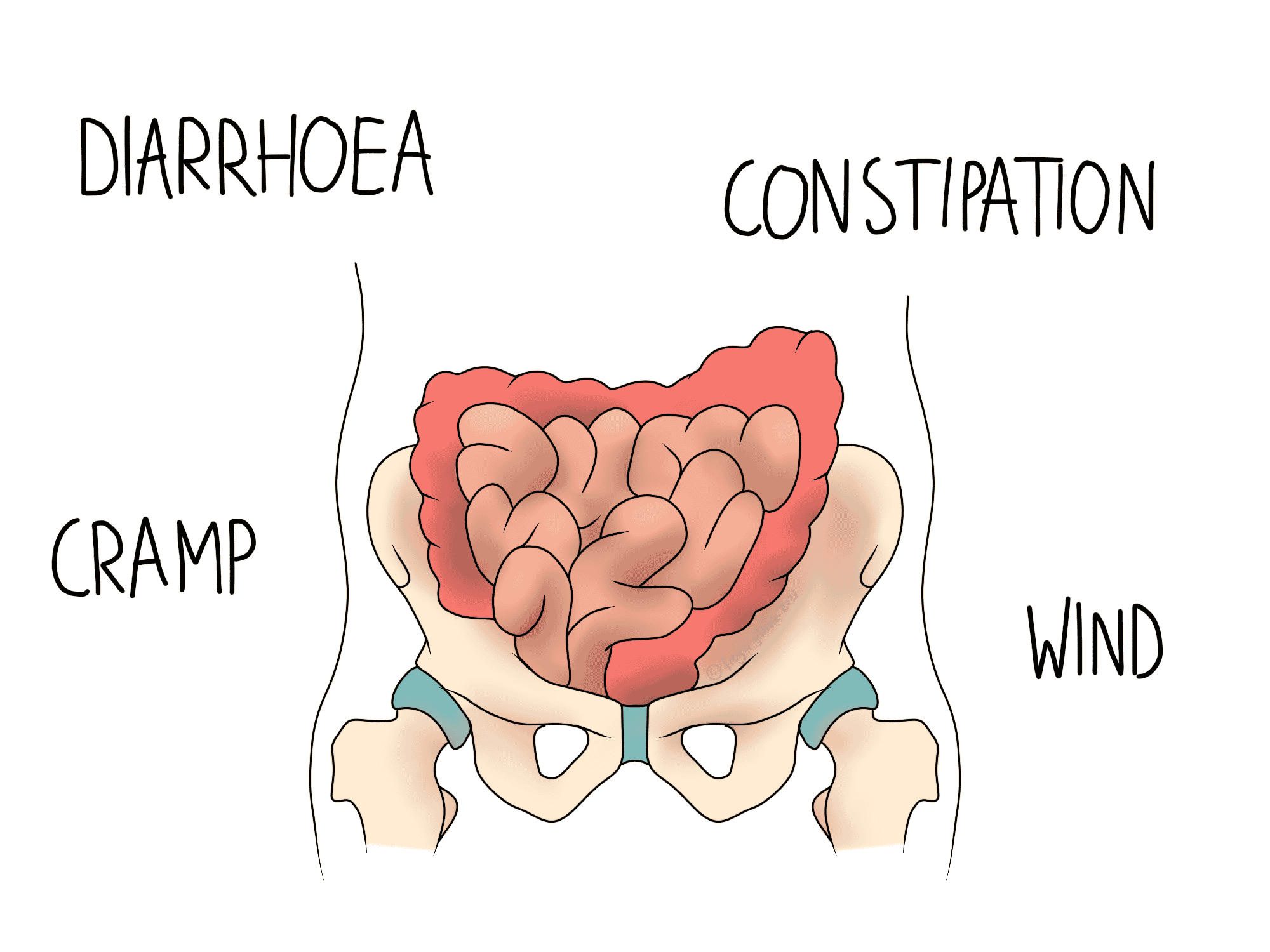
IBS stands for irritable bowel syndrome, which is characterised by episodes of diarrhoea and constipation, cramp, and wind. You may also suffer bloating and abdominal pain.
Diagnosing IBS
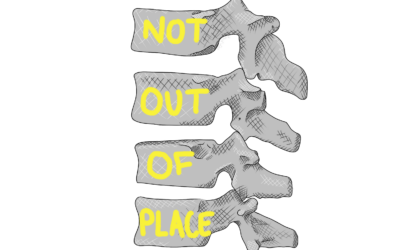
As the symptoms of IBS are so broad, they could well be a sign of something else. There is no single test to diagnose IBS, and instead the diagnosis should be made in the absence of diagnosis for another condition. This means that tests for things like Crohn’s disease and Ulcerative Colitis should be conducted first. These two conditions come under the umbrella of IBD, which stands for inflammatory bowel disease. IBD can have a rheumatological component, which can impact the musculoskeletal diagnoses your osteopath will consider if you’re presenting with other aches and pains. For example, ankylosing spondylitis (AS) is a rheumatological lower back condition that often looks a lot like non-specific (“normal”) lower back pain. However, a personal or family history of IBD makes AS much more likely to affect you, so it would help for us to know if that applies to you.
Mechanisms and Triggers of IBS
The symptoms of IBS can flip from one end of the scale to the other. Alternating constipation and diarrhoea are associated with the excitability of the muscles in the intestines. When the muscles are over-excited, they move bowel contents through quicker, causing diarrhoea. When they are under stimulated, movement slows down and you become constipated. Both of these scenarios can cause abdominal pain, which in turn can lead to muscle and joint pains elsewhere. Abdominal pain, even when mild, can cause you to subconsciously take on a more hunched posture. This is not a problem when the position is taken on briefly, but over time it can cause some areas in the back to overwork, and others to become stiff. Your osteopath can work to relieve the aches and pains associated with this.
It is usually unclear why IBS develops in the first place, but understanding the triggers that provoke your symptoms is key to management. Often stress will encourage a flare-up, as will some foods and drinks. Keeping a symptom and food or lifestyle diary can help you to identify these triggers.
Your Osteopath’s Role
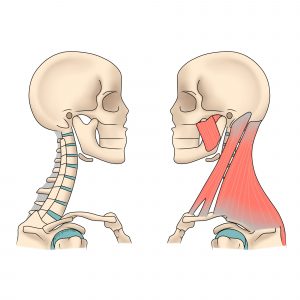
As mentioned above, IBS can cause problems for the musculoskeletal system. Prolonged hunching to improve abdominal pain is somewhat similar to the position you might take when sat at a desk all day. In clinic we often see desk workers with stiff upper backs, overworked lower backs and necks, and tight chest muscles. These in turn can lead to headaches, thoracic outlet syndrome, and lower back pain.
One study has suggested that manipulation (clicking) of the mid and lower back could help to relieve some symptoms of IBS. A theory to explain this is that the excitability of the intestines may be associated with unusual nerve activity. Clicking a spinal joint typically improves movement in the joint, but may also have a local effect on muscles and nerves. By manipulating the level at which the nerves supplying the bowel leave the spine, it may be possible to influence bowel function.